A series of significant failings were made in the care of two vulnerable patients who died at an NHS mental health trust in Essex, the Parliamentary and Health Service Ombudsman (PHSO) has said.
In a highly critical report, the PHSO said the former North Essex Partnership University NHS Foundation Trust (NEP) had “missed opportunities” to ensure the safety of the young men.
The ombudsman said the men and their families had been “badly let down” by the Trust, which had failed to make improvements in the years following their deaths.
“It appears there was a systemic failure to tackle repeated and critical failings over an unacceptable period of time,” the report said.
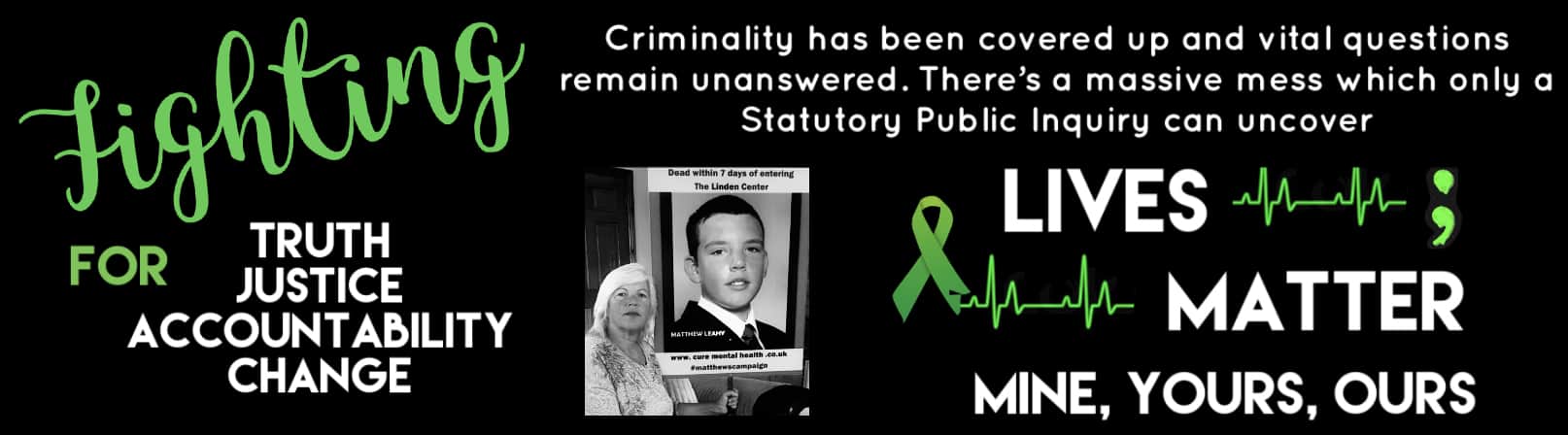
The PHSO investigated the death of 20-year-old Matthew Leahy, who was found hanged at the Linden Centre mental health unit in Chelmsford in November 2012.
It also looked at the case of another man, identified only as Mr R, who died at the unit in December 2008.
In its report published on Wednesday, the PHSO found that NEP had not adequately planned its care for Mr Leahy, who had previously been diagnosed as having delusional disorder.
He was also not adequately observed, did not have an allocated keyworker and there was an inadequate response when he reported being raped, the report said.
The PHSO said NEP’s own investigation into Mr Leahy’s death was not robust enough and found the Trust was “not open and honest” with his family about steps being taken to improve safety at the Linden Centre.
The Ombudsman also concluded that NEP did not adequately respond to Mr R’s threats to harm himself, failed to adequately manage his ward leave and did not properly assess and manage risk.
Parliamentary and Health Service Ombudsman Rob Behrens said: “These vulnerable young men and their families were badly let down by North Essex Partnership Trust.
“The lack of timely safety improvements following their deaths is completely unacceptable and it’s important the NHS understands why this happened and what lessons can be learned to prevent the same mistakes happening again.”
Mr Behrens said he was pleased that NHS Improvement, the body that oversees NHS Trusts, had accepted a recommendation to launch a review into what happened at NEP.
In a statement Mr Leahy’s parents, Melanie and Michael, said his death had “left a void that nothing can fill”.
“Not a day passes when we do not miss him and despair at the thought of how his life was cut short, so needlessly,” they said.
“Our son was ready to go travelling and celebrate his 21st birthday. He should never have died.
“Sectioned under the Mental Health Act, he was alone, scared and failed in the most appalling way by those entrusted with his care.
“We want the public to know what happened to our son so this never happens again.”
Following the Ombudsman’s investigation into Mr R’s case, the Trust paid his family £1,250 in recognition of the distress caused, wrote to them to formally apologise and set out the action taken to improve its services.
The PHSO also recommended that within two months the Trust should send a written apology to Mrs Leahy and pay her £500 for the distress caused by the receipt of inaccurate information about safety changes in February 2015.
As part of its investigation into Mr Leahy’s death, the Ombudsman developed a timeline of evidence of systemic failings to address issues of patient safety at NEP from December 2008 onwards.
Its report drew on the findings from a Coroner’s inquest, a number of critical Care Quality Commission (CQC) inspection reports and criticisms by Essex Police.
In November last year, police dropped an investigation into up to 25 deaths at NEP-run facilities since 2000.
Investigators found “clear and basic failings” in care, but insufficient evidence for corporate manslaughter charges.
A Health and Safety Executive (HSE) investigation into how NEP managed its mental health wards is still ongoing, with the Ombudsman saying there remained a “possibility” of criminal charges being brought against the Trust.
In April 2017, NEP merged with the South Essex Partnership University NHS Foundation Trust to become the Essex Partnership University NHS Foundation Trust (EPUT).
The EPUT receiving a good rating from the CQC in its latest inspection in 2018.
EPUT chief executive Sally Morris offered its “deepest sympathies” to the families of the “beloved sons” who died under the care of NEP.
She added: “The Ombudsman reports that, in both these cases, the care by the former NEP fell well below acceptable standards, let alone the high quality of care the NHS strives always to provide, and this has caused deep distress to their bereaved families. Our hearts go out to them.
“It is also evident from the report that the former Trust’s investigation into Matthew Leahy’s death was inadequate.
“We are very sorry indeed for the additional pain and distress this has caused Mr and Mrs Leahy.”
She added: “We will carry out the Ombudsman’s recommendations and will support NHS Improvement’s forthcoming review into the former NEP in every way possible.”
https://www.heart.co.uk/essex/news/local/significant-failings-at-former-essex-nhs-trust/