Judge says Essex Partnership University NHS foundation trust had failed to prevent suicides
An NHS mental health trust has been fined £1.5m over serious lapses in care that led to the death of 11 patients who were found hanging.
Mr Justice Cavanagh, the judge who imposed the fine, said a “litany” of failings in safety standards had been identified at Essex Partnership University NHS foundation trust (EPUT) over many years, which meant that it had failed to “prevent suicides”.
The fine relates to 11 deaths in which a “point of ligature was used within the ward environment of the trust’s premises” between 1 October 2004 and 31 March 2015.
EPUT pleaded guilty last November to an offence under the Health and Safety at Work Act 1974 in a prosecution brought by the Health and Safety Executive (HSE). The judge imposed the £1.5m fine in a sentencing hearing on Wednesday at Chelmsford crown court.
Paul Scott, the trust’s chief executive, apologised to the 11 families involved and said: “I am fully committed to ensuring that every lesson is learned.” The trust has spent £10m in the last year to improve safety on its wards, he added.
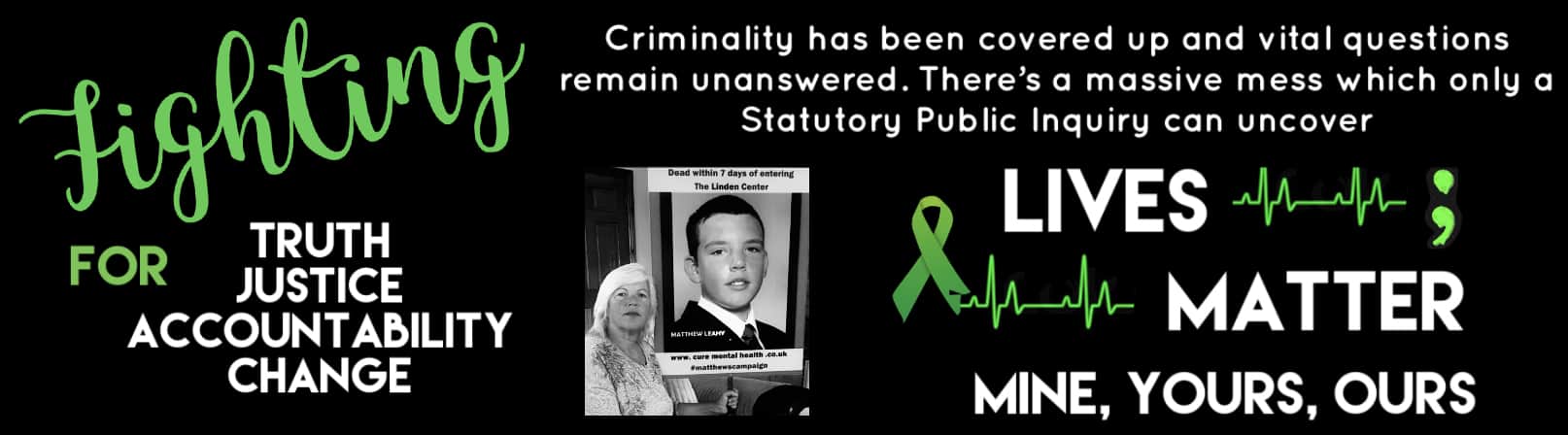
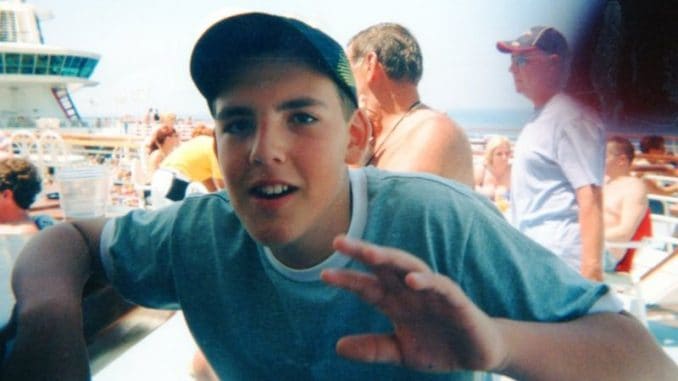
But Melanie Leahy, whose 20-year-old son Matthew died at the Linden Centre in Chelmsford, which looks after men with acute psychiatric problems, said the HSE prosecution “means nothing”.
The fine is the latest setback for the trust, which is the subject of an ongoing public inquiry into how scores of patients came to die in NHS mental health facilities across Essex between 2000 and 2020.
The government set up the inquiry, which is being chaired by the psychiatrist Dr Geraldine Strathdee, in January. It was established in response to claims over vulnerable patients dying as a result of receiving inadequate care and being poorly supervised while undergoing residential treatment.
Strathdee has pledged to find out why patients died and acknowledged “the intolerable pain and loss that the families of those who died have experienced”. Her inquiry is due to report in spring 2023.
However, a group of families of 67 patients who died or suffered serious mistreatment while undergoing mental health care in Essex have criticised Strathdee’s appointment because she was previously the NHS’s national clinical director for mental health in England.
In a statement in March, the families said that the inquiry would not be able to uncover the full truth of how their loved ones came to die because, as a non-statutory inquiry, it cannot compel witnesses to attend and give evidence under oath. Solicitor Priya Singh, of Hodge Jones & Allen, the families’ lawyers, said that the inquiry would be “toothless” as a result.
In January, the Care Quality Commission told EPUT to improve the safety of the care it provides after an inspection uncovered lapses which posed a risk to patents including the absence of staff who were meant to be observing inpatients and staff not doing what they should to maintain safety.